In 1971, US president Richard Nixon declared war on cancer, and the US Congress supplied significant financial ammunition with the signing of the Cancer Act. In the intervening 47 years, countless millions of dollars have been spent in the US and all around the world on research into the disease. Yet it remains a major killer, and among the most feared of all human pathologies.
Moreover, regardless of the veracity of double Nobel prizewinner Linus Pauling’s supposed quote about most cancer research largely being a fraud, there is no denying that the field has become caught up in concerns about the reliability of scientific research papers more generally.
In 2011, researchers from the pharmaceutical company Bayer HealthCare published a paper in Nature reporting that they had been able to replicate only between 20 and 25 per cent of 67 published preclinical studies, mostly in cancer. The following year, another Nature paper revealed that researchers from Amgen had been able to reproduce just six of 53 “landmark” cancer studies. “Clearly there are fundamental problems in both academia and industry in the way such research is conducted and reported,” the firm’s paper concluded.
Since then, a major project attempting to reproduce the findings of other major cancer papers, the Reproducibility Project: Cancer Biology, has had mixed results: of the 10 studies completed since 2013, only five were mostly repeatable, while three were inconclusive and two were not repeatable. Moreover, at the end of July, the project’s leader, Tim Errington, announced that the initial target to reproduce 50 papers had now been downgraded to only 18, due in part to their lack of methodological detail.
Meanwhile, public confidence was no doubt further undermined by front-page allegations of research misconduct against prominent Ohio State University cancer researcher Carlo Croce, published in The New York Times in March 2017 (Croce disputes the allegations and is reportedly suing the newspaper). Another star Ohio State cancer researcher, Ching-Shih Chen, resigned earlier this year amid multiple findings of research misconduct against him.
So is cancer research on the right track, both scientifically and structurally? Could the amount of public, private and charitable funding poured into it actually be a hindrance, encouraging sloppy and sharp practices, wasteful duplication and exaggeration of findings? Or has cancer research achieved more than anyone could have ever dreamed of, given how complicated the disease has turned out to be? Was Nixon’s war on cancer the scientific equivalent of Vietnam? Or is it more like a very long world war, whose multiple front lines are all slowly but surely inching forwards as understanding and technology advances?

‘Putting a man on the moon was an engineering problem, but cancer remains primarily a scientific problem’
As a cancer researcher, I am frequently asked when the disease will be cured. In truth, I ask myself the same question every day.
In the 1980s, I was a physician, and I saw at first hand how cancer devastated my patients and their families. In the 1990s, I became a laboratory-based researcher, convinced that we needed a much deeper understanding of cancer if we were to develop better treatments.
In 2003, my wife, a celebrated breast cancer surgeon, underwent surgery, chemotherapy and hormonal therapy for an early stage breast cancer that she had self-diagnosed between two operating room cases. Although she survived, her chemotherapy caused neurological toxicity that prevented her from returning to the profession she loved. In 2010, she developed a malignant brain tumour, unrelated to her breast cancer. Despite surgery, state-of-the-art radiotherapy and other medical interventions, it killed her five years later. I share the frustration that progress against cancer has not come faster, especially given the resources that have been marshalled against it for decades.
In thinking about cancer, it is helpful to understand some of the differences between science and engineering. Scientists produce new knowledge, and engineers apply that knowledge. In 1960, President Kennedy challenged us to put a man on the moon within a decade. In 1971, President Nixon declared a war on cancer. While the former led to the successful lunar landing in 1969, the war on cancer continues.
But putting a man on the moon was an engineering problem, thanks to scientists such as Galileo and Newton. That is why it lent itself to a timeline, with stipulated deliverables. I understand the urge to regard cancer as an analogous case, solvable by simply reorganising the research community and resourcing it appropriately. But it isn’t. Cancer remains primarily a scientific problem.
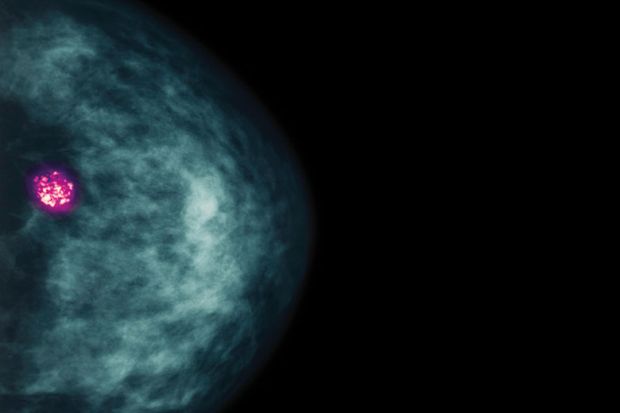
For example, we now know that cancer is caused primarily by the accumulation of DNA alterations (mutations) in particular cells in the body. The first draft of the normal sequence of human DNA – needed to systematically identify these mutations – did not appear until 2000. Only then did this particular battle in the war on cancer become an engineering problem: how to make routine DNA sequencing affordable. That has now been achieved, and it has revolutionised diagnosis. But it is only the first step on a long road towards treatment.
Scientists still have to learn how, mechanistically, each mutation contributes to the misbehaviour of cancer cells and the tractable vulnerabilities that it imparts upon them. Making matters worse, cancer-causing mutations have been identified in hundreds of different genes. Furthermore, unlike single-gene disorders such as sickle cell disease or cystic fibrosis, cancers are typically caused by the accumulation of multiple mutations acting in concert, much like the tumblers of a lock falling into place, and no two cancers have the same combination of mutations. Even the cells within the same tumour can create genetically distinct progeny that serve as a reservoir for treatment-resistant variants. While an increasing number of cancers are now treatable, too many remain intractable. More knowledge about basic cancer biology is imperative before engineering can truly take over.
Such discovery science – especially the type that fundamentally changes the way we think about a problem – is often driven by creative individuals who have been allowed to follow their curiosity. Scientists should be held accountable for the resources they are given, but forcing them into teams and holding them to a predetermined schedule for breakthroughs risks creating a herd mentality inimical to heretical, transformative thinking. The next big advance in, say, breast cancer might come from someone studying breast cancer, but it could also come from a basic scientist studying fundamental biological mechanisms in a model organism such as the fruit fly or the worm. And it may come tomorrow, or it may come 20 years from now.
This is why the pharmaceutical industry relies on the public sector, including governments and philanthropic organisations, to fund early stage discovery science, which is typically conducted in academic laboratories; most companies cannot justify investments in open-ended, curiosity-driven discovery science to their investors. Linking academic research funding to perceived clinical utility not only threatens this symbiotic relationship but also has other unintended consequences. For example, some of the problems with the irreproducibility of published scientific papers almost certainly stem from basic science investigators being coerced, by funders and publishers, into conducting applied science experiments that they are poorly trained to perform.
Knowledge, like art, is one of the greatest gifts we can give to future generations, and it is clear that the more we invest in discovery science, the faster we will generate it. But the fruits of that knowledge cannot be predicted in advance. For the benefit of all the stakeholders involved in cancer research – most importantly, patients and their families – we must acknowledge this, instead of overpromising that investments in science will transform care in the short term.
William G. Kaelin, Jr is the Sidney Farber professor of medicine at the Dana-Farber Cancer Institute, Harvard Medical School, and a Howard Hughes Medical Institute Investigator.
‘Some prominent scientists have built their careers based on questionable practices’
The “War on Cancer” is of a similar vintage to the “War on Drugs”, and is often seen as having had a similar lack of success. The two do share a common naivety, but the progress of cancer research has produced important achievements that attempts at drug prohibition have not.
The perception that 47 years of huge investment in cancer research has resulted in failure stems from a number of factors, and several of these have ethical bases.
First, it is deceptive to talk about cancer as if it were one disease. There is no such thing as cancer. There are cancers. Each type is its own disease, with a distinct aetiology, rate and mode of progression, and mortality level. Human papilloma virus (HPV)-positive head and neck cancers are completely distinct from HPV-negative head and neck cancers, and they require different treatment regimens. Breast cancer is, in fact, a large ensemble of diseases, each requiring its own approach.
In many cases, moreover, it is the metastasis of the tumour that is fatal. If the media, physicians, government officials or charities obscure these issues, they improperly prevent patients and the public from truly evaluating options and progress.
Let us consider the early detection of cancer. There is no doubt that surveillance can save – or at least prolong – lives in the cases of particular cancers. Nevertheless, not all early warning technologies are created equal. Some should be provided only to members of particular risk groups. Some predominantly produce unnecessary interventions. It is not sufficient to demonstrate that some technology might “save lives”. A Swiftian could argue that one could prevent virtually all deaths from breast and ovarian cancer simply by removing all breasts and ovaries from women at puberty. This preposterous solution dramatises the necessity of balancing risks and benefits of early detection and consequent interventions when considering the population at large. On the other hand, BRCA1- and BRCA2-positive women should strongly consider surgery as life-saving early in adulthood.
The success of immunotherapies (full disclosure – I was a recipient of a Cancer Research Institute postdoctoral fellowship) in the treatment of certain cancers has highlighted another underappreciated contemporary issue. As people are surviving longer with cancer, or are being cured, the question arises of what the long-term effects of cancer treatments are on the health of patients. Long-term follow-up should be included as an integral part of both standard approaches and modern interventions, such as gene-therapy and gene-editing technologies.
Private foundations play an important role in promoting cancer research and prevention. Nevertheless, at least one organisation has been accused of being, in essence, a corporation masquerading as a charity, with high administrative costs and executive salaries, advertising campaigns purporting to be educational activities, an incessant pursuit of corporate sponsorships, an obsession with pressing claims of perceived trademark violations, and comparatively small contributions to research and treatment.
Corporate sponsorship of oncological research and licensing of intellectual property produced by government or academic institutions is fraught with ethical issues. These institutions should negotiate not only to protect their own intellectual or economic rights; ethics demands that one future condition for collaboration with industry should be that access to the fruits of the research be provided to the public equitably and affordably.
The influx of money into cancer research from both government and corporations has been a challenge to scientific integrity. One need only think of the immorality of working with the Council on Tobacco Research – the industry-funded body that lavished grants on scientists willing to cast doubt on the link between smoking and cancer – to appreciate how money and the resulting conflicts of interest can distort the reporting and interpretation of results.
The financial and career-advancement incentives for unfairly profiting from the work of others and violating scientific norms have proved too powerful for a number of cancer researchers. Some prominent scientists have built their careers based on questionable practices, and institutional responses have often been deficient. The scientific community must take these problems seriously and exert more effort to solve them.
Nevertheless, the investment in oncological research has produced immense benefit. Some of these extend beyond oncology itself. One example is the studies of peculiar viruses – now called retroviruses – that caused tumours in chickens and mice (animal experiments have been and will continue to be indispensable for progress in cancer therapy): this led not only to the discovery that cancer results from genetic alterations, but also to the development of highly effective HIV treatments (antiretroviral therapy).
It is clear that certain kinds of cancer could be greatly reduced by lifestyle changes. Most lung cancer can be prevented by not smoking tobacco. Most cervical cancer (and probably most HPV-positive cancers) can be prevented by vaccination for HPV. Needle-exchange programmes can suppress transmission of hepatitis C and the consequent elevated risk of hepatocellular carcinoma. It is clear that one should avoid tanning beds and excessive exposure to the sun. And the evidence suggests that reducing obesity would lower the prevalence of a number of cancers.
But the diversity of cancers means that any specialised diet- or supplement-based regimen or pseudoscientific “therapy” has precious little chance of providing meaningful protection. Its progress can sometimes be frustratingly slow, but scientific research will continue to provide the only means of progress towards the discovery of both prevention approaches and treatments for the diversity of human cancers.
David A. Sanders is an associate professor in the department of biological science at Purdue University.

‘It is incumbent on journalists, press officers and scientists to nurture a spirit of cautious optimism’
Forty years after the infamous “War on Cancer” was declared by Richard Nixon, cancer experts met at the World Oncology Forum in 2012 to consider whether that war was being won.
Four decades is a considerable duration for a war, and one ought to expect either a declaration of victory or defeat by this point. The cancer researcher Douglas Hanahan, Merck Serono chair in oncology at École Polytechnique Fédérale de Lausanne, highlighted the tremendous progress that had been made, such as remarkable insights into the complex molecular mechanisms of how diverse cancers develop. Still, there is a consensus that we are not winning the war, and part of the problem is that when faced with such complexity and diversity, it becomes difficult to clearly define the enemy and delineate the aims of combat.
Are cancer cells the primary enemy? Or is it the immune cells that fail to eliminate them? Or perhaps the environmental and lifestyle factors strongly associated with the increased risk of cancer, such as smoking? And will the war be won only when cures are developed for all cancers, or can we reasonably claim (intermediate) victories when prevention and treatment strategies for selected cancer types demonstrate major successes?
Hanahan advocated for a redefined, distinctly modern conception of war. For him, what is needed is a comprehensive “battlespace strategy”. This would involve concerted preventive efforts and also an understanding of the individual genetic and molecular landscape of each battle in each individual patient; such detailed knowledge would allow individualised plans of attack to be drawn up to not only tailor treatments but also marshal the body’s own resources, such as the immune system, against the cancerous enemy within.
A more recent metaphor, introduced in 2016 by the Obama administration and spearheaded by the former vice-president, Joe Biden, is that of a “Cancer Moonshot”, a major investment in cancer research with the goal of improving prevention and treatment. But while this metaphor invokes boldness and determination, it also sets up certain expectations in the minds of the public. Our planet has only one moon, whereas there are more than a hundred types of cancer; just like the “war on cancer”, the “moonshot” metaphor may subliminally convey a simplicity that does not do justice to the complexity of the disease.
We need to communicate goals and results of biomedical research in a manner that sets up realistic expectations and does justice to the nature of research progress. Cancer prevention – which has been one of the most successful strategies in the “war” – will not suddenly shoot straight up into the stratosphere, but will continue to improve over decades in slow, incremental steps. Unfortunately, there is a tendency among researchers to exaggerate the impact of their research. Institutions’ press releases use hyperbolic expressions such as “breakthroughs” or claims to have identified the “Achilles heel” of cancer. And some journalists often fall prey to this hype: a recent survey of newspaper reporting found that there was a growing trend to downplay the uncertainty inherent in scientific studies, especially when new research findings have not yet been replicated.
The public might well be bemused by the fact that, amid all these supposedly groundbreaking advances, cancer remains such a big killer. It is incumbent on journalists, press officers and scientists alike to nurture the spirit of cautious optimism that cancer patients – and all of us who are at risk of becoming one – need to hear.
Over the past decade, cancer researchers have been especially concerned by the fact that some experiments published in highly regarded research journals lead to inconsistent results when repeated by others. This “reproducibility crisis” in cancer research could be the result of a multitude of factors. It does not necessarily entail intentional wrongdoing: it could, for instance, reflect the complexity of cancer experiments, in which even tiny changes in the set-up, or unnoticed differences in the reagents, may change the outcome.
There are now organised efforts to assess which cancer research findings can indeed be repeated. So far, the results of this “reproducibility project” have been mixed. But hopefully the scrutiny that the issue is receiving will ultimately lead to greater reproducibility – and a stronger likelihood of developing new cancer treatments that work more consistently.
Jalees Rehman is professor of medicine and pharmacology at the University of Illinois at Chicago.
‘I have no reason to believe that cancer researchers are any better or worse than any other scientific research population’
In cancer treatment, we are entering a new and exciting era. The drugs that have been used for decades do not discriminate between cancer and normal cells. They kill any cell that is dividing; they work because more of the cancer cells are dividing, and those cells do not recover between treatments, as normal cells do. But plenty of damage is still done to normal cells as well, leading to the well-known side-effects of standard drugs.
The latest treatments, however, kill cancers by targeting defective genes and their proteins, which are found specifically in the cancer. Another major advance is the discovery of proteins that stop the body’s own immune cells from killing cancer cells: this means that those proteins can be disabled, allowing the immune system to do its work.
Even before these developments, however, better treatments and earlier detection of common cancers, such as cervical, breast and bowel cancers, had improved survival rates. Quoting Australian figures for 2009‑13, individuals with cancer have a 0.68 chance of living for another five years compared with the general population. Between 1984 and 1988, that figure was 0.48.
Given that progress, why are there questions about the return on cancer research investment since Nixon declared war on cancer?
First, the expectation of being able to cure cancer in one Neil Armstrong-style giant leap for mankind was unrealistic. Cancer is actually more than 100 different diseases, and being able to identify the nature of these conditions required multiple new technologies (such as tools to identify the cancer genome). Treatment improved, but in small steps. There was to be no magic bullet (or rocket).
The success achieved does not mean that resources could not have been better allocated. Progress in research can be driven by both competition and collaboration. If that balance is skewed too far towards competition, groups can be unnecessarily replicating the work of others.
Another issue is that common cancers attract more research funding than rarer cancers. Success with a common cancer attracts new researchers to that field, again increasing the chance of overlapping research programmes. Also, there are sufficient patients to enable clinical trials of new agents, and pharmaceutical companies are likely to have a higher return on investment if a successful therapy will be used by a larger population. Even governments can be tempted to concentrate funding on research that is likely to achieve the greatest good for the greatest number. But ideally, that instinct should be balanced by a recognition of a responsibility also to ensure that those with rare cancers are not forgotten.
The cancer research community is a microcosm of society. There can be strong temptations for the morally weak in the multibillion-dollar rewards for successful anti-cancer therapies, as well as in the academic and grant-winning success that comes with prominent publications: something that, again, is relatively easy to achieve in the oncological field, given cancer’s high profile, provided that you can present an eye-catching finding. But this high profile is a double-edged sword: those cases of corrupt behaviour that occur are often highlighted by the popular press.
Outright corruption remains rare. But there are more subtle levels of misconduct than falsifying results or plagiarising others’ work. The interpretation of results can be subject to “spin” that attempts to promote a modest improvement in outcome up to the level of a major breakthrough and a new standard of care, in order to encourage its uptake.
Still, I have no reason to believe – or data to suggest – that cancer researchers are any better or worse in this regard than any other scientific research population. Apart from anything else, cancer research covers a broad range of disciplines, from laboratory researchers to clinicians – including those in allied health.
The majority of researchers in all these fields have a passion for what they do, and are prepared to tolerate the uncertainty of living from grant to grant – and perhaps never achieving public recognition – in order to make their contribution to this most vital of research fields.
Ian Olver is professor of translational cancer research and director of the University of South Australia Cancer Research Institute.
 Source: Getty
Source: Getty

‘Soon clinicians will be able to tailor, combine and adapt therapies to each individual patient’
Marie Curie said: “One never notices what has been done; one can only see what remains to be done.”
Most cancers are diseases of age. Over time, DNA accumulates mutations that escape the body’s repair machinery. According to the National Cancer Institute, 77 per cent of all cancer cases in the UK are diagnosed in people of age 55 and over, while people of 65 years or over account for more than half of all cancers diagnosed. The reality is that as we combat other diseases and improve our life expectancy, we also live long enough to increase the chances of developing cancer. Hence, at least half of us will develop cancer at some point in our lives.
But a statistic that is rarely noticed is that 50 per cent of cancer patients survive free of disease for 10 years or longer, according to Cancer Research UK. These rates are much higher in the most common cancers: 78 per cent in breast and 84 per cent in prostate cancer patients. In the past 40 years, survival rates have doubled in the UK.
Thanks to advances in genome sequencing, medical imaging and other technologies, we now have a deeper understanding of many cancers than we could have imagined. What’s more, this understanding is resulting in smarter therapies that are directly benefiting patients. For example, radiotherapy can cure more than 90 per cent of localised prostate cancers. The i-Knife, a novel surgical device, “smells” tumour cells and guides the surgeon to remove more of the tumour and spare the healthy tissue. Meanwhile, radiotherapists are developing the MR-Linac, an integrated device that will take images of the patient and adjust the therapeutic radiation beam in real time to focus on the tumour and avoid healthy organs.
Importantly, sequencing cancer genomes from tens of thousands of patients continues to deepen our understanding of many cancers. In 2002, through collaborative efforts, a mutation in a gene named BRAF that drives most melanomas was discovered. Nine years later, the drug vemurafenib was approved, providing treatment for a cancer whose patients were previously without hope. A recent analysis of approved drugs in which I was involved showed that oncology was the disease area with the greatest number of novel drugs approved.
It is also clear that the greatest ground has been made up in common cancers, on which we have been able to amass the largest amounts of data. For the remaining half of cancer patients, the picture is more complex. The precise molecular causes of many cancers remain poorly understood, and some are so rare or heterogeneous that clear patterns are difficult to ascertain. Moreover, many patients may initially respond to drugs but later develop resistance, much like we see with antibiotics.
But mathematical modelling and artificial intelligence offer the prospect of analysing data from genomics, pathology and clinical imaging together, looking for hidden signals in these vast data. This could map the complex molecular communication networks used by cancer genes, identify novel drug targets and discover uses for already approved drugs outside their initial indications. AI is also helping us to map a better collective view of the patient, allowing us, for example, to better predict the risk of side-effects, informing clinicians to help them plan therapy. Importantly, AI will play a pivotal role in early detection of cancer, and the US Food and Drug Administration has approved the first AI-based software for tracking cancer.
All this will enable clinicians to tailor, combine and adapt therapies to each individual patient. Perhaps most encouragingly, cancer research is now almost entirely a collaborative, interdisciplinary endeavour. So, in our moments of doubt about the rate of progress, we must remember the amazing successes that we have achieved over the past 50 years and embrace the new technologies that will help us win the remaining battles.
Bissan Al-Lazikani is a team leader at the Institute of Cancer Research in London.
‘In a system where job security is increasingly difficult to achieve, how can we ensure that the best talent is retained so as to make greater strides in cancer research?’
Cancer is a complex disease and will require a multidisciplinary approach to truly combat it. Despite these two widely accepted facts, the overwhelming majority of cancer research funding is still spent on laboratory-based medicine and clinical trials. It strikes me that a major piece of the jigsaw is being underfunded.
As a cancer epidemiologist and population researcher, I consider cancer from the context of the person, their characteristics and their behaviours at a population level. This is not the “blame game” on an individual level, but we do know that about four in 10 cancers can be prevented. If more funding was put into preventive measures, we could make a big impact on the costs associated with cancer treatment. Indeed, one of the greatest success stories in the past decade has been the recognition of the human papilloma virus as a major risk factor for cervical cancer development. The wider benefits of HPV vaccination for prevention of some head and neck and anal neoplasms are also being recognised. And yet, more funding and support to encourage HPV vaccination is still needed, particularly for its roll-out to boys.
There also remains the challenge of applying this model to other cancer sites. I work mostly on oesophageal and bowel cancer research, where the associated risk factors of obesity, smoking, poor diet and high alcohol intake cannot be resolved through a vaccine. Investment in large-scale, public health initiatives is needed to tackle these behaviours.
In May, the World Cancer Research Fund launched its policy framework for prevention. Cancer Research UK has also recently launched a major funding stream to support research in this area. It will be several years before the impact of these schemes is seen and other similar opportunities are needed. More research on how to promote breastfeeding and tackle childhood obesity, for example, would also reduce cancer cases. However, framing this kind of work as cancer research can be a difficult sell to the fundraising public.
Other obstacles also remain. The current structure of grant funding requires reform. First, I believe we need greater recognition that people are our most valuable asset. In a system where job security is increasingly difficult to achieve, how can we ensure that the best talent is retained so as to make greater strides in cancer research? Postdoctoral research fellowships in cancer research are notoriously competitive, so alternative schemes for investing in early career researchers, rather than specific projects, should also be considered. Second, many universities, including my own, have set income targets for academics. Such models of funding targets could encourage researchers to design deliberately expensive projects. Academics are not rewarded for cost-effective research – and yet this is exactly what we should be aiming for. One of the projects of which I am most proud, which led to a very high-impact journal publication, cost nothing more than an undergraduate’s time for one year and my associated supervision time.
And, third, while the desire for novel, innovative research remains foremost when judging most grant applications, this is not always appropriate. It is only when multiple studies show similar findings that results become accepted, so we need more funding schemes such as the Reproducibility Initiative. That will not necessarily involve the most cutting-edge, new-fangled, shiny technology. There is now a mutational signature that can be analysed in tumour tissue and indicates if a patient was a smoker. Exciting, yes? Oh wait, it says in their medical record that they were a smoker.
Helen Coleman is senior lecturer in cancer epidemiology at Queen’s University Belfast.
Register to continue
Why register?
- Registration is free and only takes a moment
- Once registered, you can read 3 articles a month
- Sign up for our newsletter
Subscribe
Or subscribe for unlimited access to:
- Unlimited access to news, views, insights & reviews
- Digital editions
- Digital access to THE’s university and college rankings analysis
Already registered or a current subscriber?